There are an estimated 46.6 million people in the United States living with a mental health disorder, according to the National Institute of Mental Health. Some mental illnesses are considered minor and eventually disappear on their own, but other mental conditions are serious, and they have the ability to affect a person’s everyday life. Serious mental illnesses can make it difficult to complete simple tasks, like going to work, doing the laundry, and getting quality sleep.
But regardless of the type of mental illness—whether it’s OCD, depression, or an eating disorder—getting treatment is important. When a mental illness is addressed early on, it significantly reduces the risk that a person will find themselves facing more serious situations down the road, like suicide or addiction.
When we think about treatment for conditions like depression, it’s easy to assume that anyone who visits a therapist or takes antidepressants will improve. But what happens when someone seeks treatment for depression, and they don’t get better? It’s called treatment-resistant depression, and it’s actually more common than you think.
The Trouble With Treatment-Resistant Disorders
Research shows that about one-third of adults with depression have a specific condition that does not improve with treatment. A depressive disorder is generally classified as treatment-resistant if a patient has not responded to the correct dosages of two different antidepressants for roughly six weeks. It doesn’t take into account other forms of treatment, such as talk therapy, holistic medicine, or non-invasive procedures. Obsessive Compulsive Order (OCD) is another mental illness that can become treatment-resistant.
Of course, many therapists will do everything in their power to help someone who is struggling to find a successful treatment. Psychiatrists might keep a patient on one medication for longer because some drugs take more time to work in certain people than others. A therapist may also slowly increase the dosage to see if a higher potency makes a difference. It’s also common for therapists to find a combination of drugs that can work together to make a patient feel better. Sometimes, antipsychotics, mood stabilizers, or even thyroid medication can be effective for people with depression or OCD.
For people with treatment-resistant depression or OCD, it can be very challenging to accept the fact that conventional methods haven’t worked. Many people suffering from a behavioral or mental health disorder spend significant amounts of time and money finding reputable doctors to help them improve their condition. When treatments aren’t working, the feelings of frustration and disappointment can make an existing mental illness even worse.
How Family Members Can Help
If you have a family member who is struggling with treatment-resistant depression or OCD, you know how difficult it can be for them. And like all mental health disorders, it’s possible that treatment-resistant conditions can impact relationships. That’s why it’s important to have strategies for supporting loved ones while they’re dealing with treatment-resistant mental health conditions.
As a family member, make sure you’re taking the time to ask the person how they’re doing. Even if they give you the same answer every time, it’s important to show them that you are there for them and that you care about their wellbeing. Listen to them talk without jumping to conclusions or offering a solution to their problem. Just be a sounding board for them to discuss their feelings if and when they are ready. When you’re around them, try to keep it as relaxing and stress-free as possible. Plan fun activities that the person enjoys, and find ways to keep them active and out of the house.
Why Treatment-Resistant Individuals Should Try TMS
When people facing treatment-resistant depression or OCD have exhausted all their options, they often turn to Transcranial Magnetic Stimulation (TMS). TMS is a non-invasive procedure that delivers electromagnetic pulses to different parts of the brain that are responsible for mood control. In people with depression, certain regions of the brain have less activity than in healthy brains.
In a typical TMS treatment session, an electromagnetic coil is placed around the forehead. The coil painlessly delivers a pulse the stimulates nerve cells in different regions of the brain. Those sections get activated, which allows the brain to release healthy neurotransmitters. The procedure is short, completely safe, and does not require the patient to be under anesthesia. Any side effects are generally mild but could include headache or lightheadedness after treatment.
Although TMS is still a relatively new form of mental health treatment within the last 30 years, scientists have lauded its ability to improve symptoms in patients with depression and OCD. In one particular study, researchers selected 12 patients with OCD to receive TMS and then evaluated their mood eight hours later. During the evaluation, the patients showed a significant decrease in compulsive urges, especially after repetitive stimulation of the right lateral prefrontal cortex of the brain.
TMS Treatment at Pulse
At Pulse, we offer FDA-approved TMS treatment for people with depression and OCD. The process starts by meeting with our psychiatrist to determine if the patient a good candidate for the procedure. Once they’re approved, we create a treatment schedule—we recommend daily, 18-minute treatments for about 6-8 weeks. Our therapists will also talk about additional treatments that will work in tandem with TMS. All procedures are done in our beautiful offices in Los Angeles and Santa Barbara, and we accept most major insurance plans.
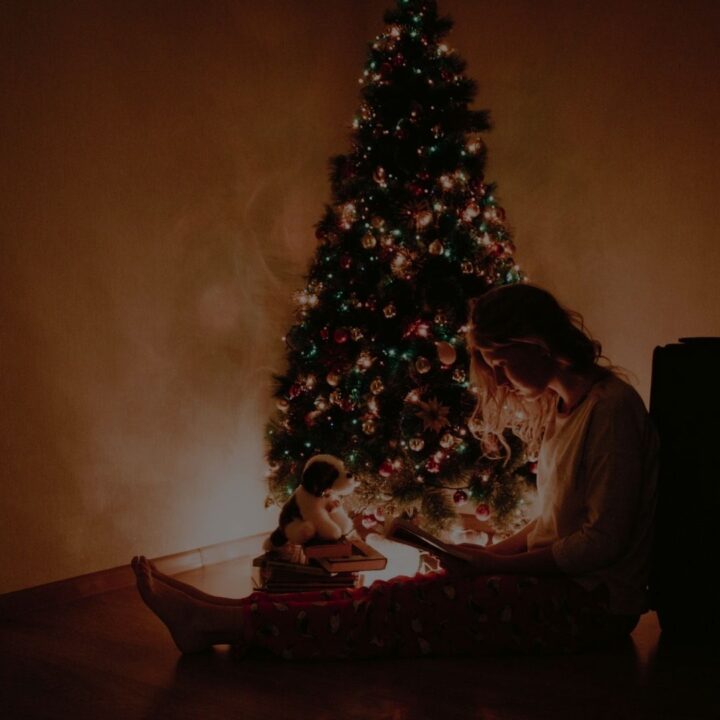
With the holidays around the corner, now is the perfect time to give your loved ones the gift of TMS. Encourage them to try TMS so they can start the new year off on the right foot, feeling their best. Contact us to learn more about TMS at Pulse.

