The Correlation Between Major Depressive Disorder and Genetics
Major depressive disorder is one of the leading causes of disability worldwide.
Major depressive disorder is one of the leading causes of disability worldwide. More than 18% of all adults in the U.S. will be diagnosed with depression in a given year. For Americans aged 18 to 44, major depressive disorder is the third most common cause of hospitalization. People with untreated depression are at high risk of self-harm and suicide, and they are also at risk of turning to drugs and alcohol to cope. For people with depression symptoms, it is critical that they get help for their disorder. Although depression is common and the symptoms debilitating, there are numerous and effective treatment methods for depression.
While it’s true that anyone can develop a mental health disorder like major depression, there are several risk factors and protective factors that impact symptom manifestation. Genetic risk factors are correlated with major depressive disorder manifestation, and people who have a family history of depression may be at higher risk of developing the disorder than those who do not possess genetic markers for the disease. Fortunately, people in high-risk brackets for depression can take several steps to lower their chances of experiencing depression symptoms. Just because an individual may have a close relative with the disorder does not mean that they are doomed to experience the same issues.
What is major depressive disorder?
Depression is an umbrella term for a range of depressive disorder subtypes. While the disease itself is difficult to endure, it also raises a person’s risk for other health issues such as heart disease and dementia. Depression symptoms can manifest differently for each patient. The most common types of depression disorders are major depressive disorder, dysthymia, bipolar depression, and seasonal affective disorder or SAD. Also, women are at higher risk of developing a depressive disorder than men. There are specific clinical subtypes that are unique to women, including PMDD, and perinatal and postnatal depression. The different subtypes of depression also have different triggers for the disorder. For example, extreme changes in weather patterns that persist can trigger SAD. Most people with SAD will develop the disease during the dark, dreary winter months. But a minority of patients will experience SAD during spring and summer.
In major depression, the state of hopelessness, guilt, and low-self worth is an all-consuming feeling that is also characterized by a marked loss in pleasure and motivation. Episodes of major depression can last as little as two weeks to several months. People who experience one event of depression and are not treated for the disorder are at increased risk of recurrence and experiencing longer, more drastic episodes in the future. The symptoms of major depressive disorder include the following:
- Feelings of shame and worthlessness
- Excessive guilt
- Fatigue
- Trouble falling asleep or staying asleep
- Sleeping too much
- Eating too much or too little
- Changes in weight and appearance
- A lack of emotion and pleasure (anhedonia)
- Increased irritability and agitation
- Failure to uphold responsibilities
- Unable to complete their usual daily tasks
- Slowed speech and movements
- Random aches and pains
- Drug and alcohol use
- Self-harm
- Suicidal ideation and attempts
Many of the symptoms of major depression can also contradict each other. For example, some people with the disorder may sleep way too much, while others won’t be able to sleep.
Depression patients may also become listless and experience a lack of emotion, while others will become emotionally volatile. Major depressive disorder can also wreak havoc on someone’s appetite, causing them to either eat more than average or they may not be able to eat much at all.
Depression doesn’t just cause emotional pain and behavioral changes, either. Major depressive disorder can also cause physical pain and aching joints. The symptoms of depression can be so debilitating and distressing that many will turn to drugs or alcohol to cope with their pain. While drugs and alcohol can alleviate symptoms in the short-term, drug, and alcohol abuse worsens symptoms in the long run and can also cause people to develop a co-morbid substance use disorder. Without treatment, people with major depressive disorder can experience the consequences of the disorder for a lifetime.
What are the risk factors for depression?
While genes do play a significant role in depression symptoms, a person’s personality traits, and their environment can also cause them to develop the disorder. In cases of postpartum depression, women with no other risk factors for depression can develop symptoms thanks to significant fluctuations in hormone levels, and the stress of giving birth and caring for a newborn. When it comes to major depressive disorder, some of the most significant risk factors for developing the condition include the following:
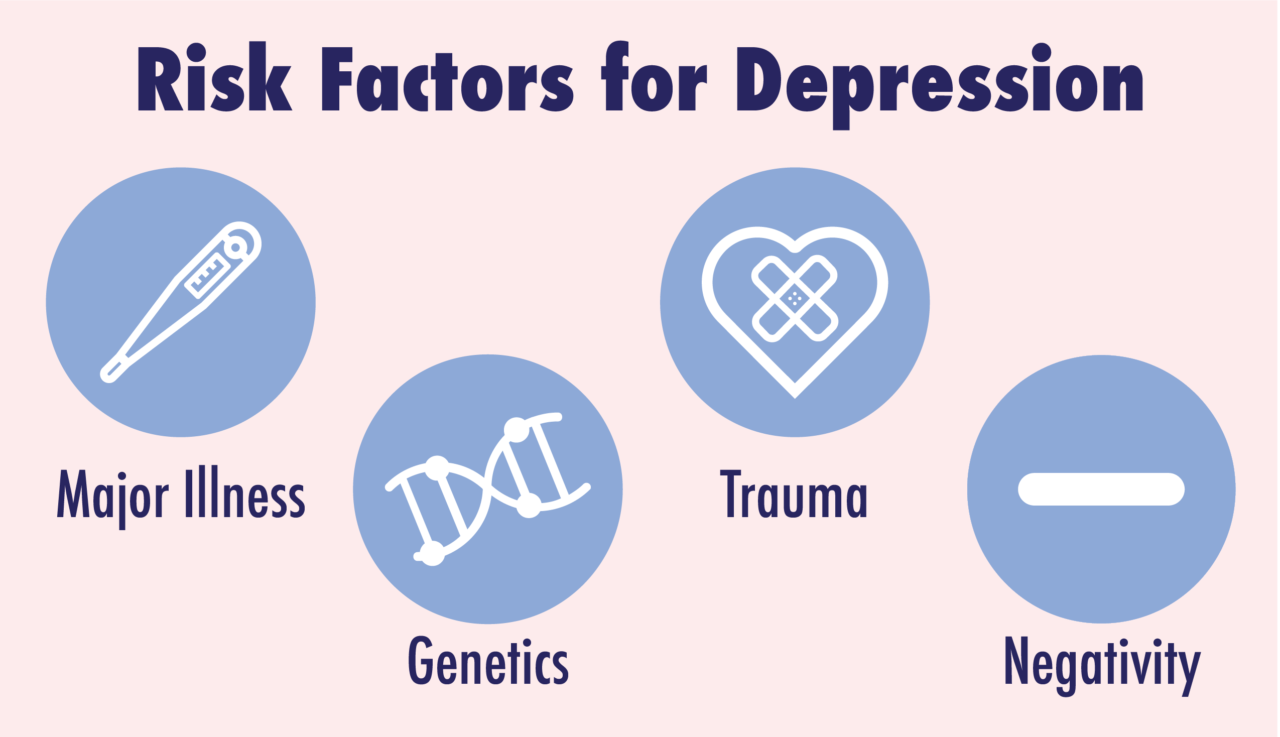
- Self Criticism and Negativity
Being self-critical or prone to a negative outlook are both inherent personality traits that can increase someone’s risk of developing major depressive disorder. Researchers from Yale and Wesleyan University found self-criticism was a significant factor in both depression manifestation and problems functioning in relationships. Further studies have uncovered that people with high levels of self-criticism, and feelings of helplessness and separation and rejection anxiety had a high risk of experiencing depressive episodes.
- Trauma
Current research supports a strong correlation between traumatic experiences and the development of depression. People who have undergone a single traumatic event and people who have been subjected to repeated trauma are both at risk of depression and also anxiety. Childhood abuse was one of the most significant risk factors for experiencing depression episodes as an adult. Studies on women with depression have uncovered that more than half of all depressed women are victims of physical or sexual abuse in childhood or adulthood. Major depressive disorder and other clinical subtypes of depression are also associated with PTSD from combat, violence, and natural disasters.
- Major Illness
Being diagnosed with a chronic, serious, or fatal disease can also increase someone’s risk of developing depression. Studies have found that up to 77% of all patients with cancer, Alzheimer’s, and AIDS have major depressive disorder. Unfortunately, many of the medications used to treat depression symptoms can interact poorly or even dangerously in people with these severe disorders, making depression even more difficult to treat for these patients.
- Genetics
The medical community overwhelmingly believes that a person’s chances of becoming depressed increase if they have a close relative with the disorder. So far, scientists have not been able to uncover one single gene for depression or a mutation that causes the illness. Some studies have suggested that depression is actually a combination of several genes that can be triggered by environmental factors to manifest depression symptoms and other mood disorders. Research conducted on twins has identified a biological component of depression. The studies on twins and depression have uncovered that having a twin with depression will significantly raise a person’s risk of becoming depressed, even if they have grown up in a different environment.
How do genetics play a role in major depressive disorder?
Scientists have determined the genetic risk factor for major depressive disorder by looking at the patterns of illness in families. This has allowed researchers to understand and estimate the disease’s heritability, or roughly what percentage of the disorder is due to genetic factors or other factors. The most reliable prediction of depression as an inheritable disorder have been found through twin studies.
In twin studies, researchers will identify a twin who has been diagnosed with major depressive disorder. An identical twin will share 100% of their genes with their other twin, while non-identical twins share half of their genes. If genes are the most significant cause of depression, then it stands to reason that an identical twin would have a higher risk factor for depression than a non-identical twin with a sibling with the disorder. In twin studies, researchers have found that heritability for depression is somewhere between 40% and 50%.
Adoption studies have also found that an adopted person’s risk of depression is more significant if one or both biological parents had depression. The current consensus on parental risk factors is that someone with a parent or non-twin sibling is anywhere between 20% and 30% at risk of developing depression than someone whose parents and siblings do not have the disorder. A person with no known genetic risk factors has about a 10% risk of becoming depressed.
In most cases of depression, the current consensus is that about 50% of depression risk is directly attributed to a person’s genes, while the remaining 50% can be attributed to non-genetic factors. Scientists are still not sure how much these percentages deviate. It is possible that an individual’s risk of becoming depressed could be 100% genetic, or their risk could not be related to genes at all. Research into the extent that genes play a role in depression is still ongoing.
In most cases of depression, the current consensus is that about 50% of depression risk is directly attributed to a person’s genes, while the remaining 50% can be attributed to non-genetic factors.
Also, the number of episodes a parent or sibling has of depression, and if their episodes started early in life can impact whether or not someone is at risk of developing the disorder too. People with a parent or sibling with recurrent depression or depression that manifested at a young age have a genetic risk factor for developing depression at four to five times the general population.
Since scientists currently believe that there is no single depression gene, people don’t merely inherit depression from either their mom or dad. Instead, depression is a known combination of genes that predispose someone to the illness, but other risk factors can also contribute to symptom manifestation. It’s also important to understand that there are protective factors against depression, too.
Can someone with genetic risk factors for depression protect themselves from the disorder?

It is possible to develop resilience to depression, and this is one of the guiding principles behind using talk therapy to reduce depression severity and relapse. The most significant protective factors against depression include the following:
- Positive Relationships
Fostering and developing positive, healthy relationships is a known protective factor against depression. Children with a genetic risk factor for depression can be spared from the illness if they grow up in a loving, supportive environment. Adults who’ve experienced childhood trauma can heal and protect themselves from depression manifestation by forming strong and healthy relationships with supportive people. Therapy can give patients the tools they need to make friends and build lasting relationships.
- A Positive Attitude
Practicing gratitude and imagining positive outcomes are associated with increased happiness and reduction in depression symptoms. Positive thoughts and gratitude have been found to increase the neurotransmitters serotonin and dopamine, which are linked to depression symptoms.
- Self-Care
Maintaining a healthy diet, exercising, and getting good quality sleep is known to prevent and lessen depression symptoms. Everyone has a different trigger for major depressive episodes, and a lack of sleep and stress are common triggers for the disorder. Studies have found that in adolescents, a lack of sleep puts them at greater risk of depression than their well-rested peers. People who struggle with insomnia and chronic sleep deprivation are at risk for major depressive disorder, too. Self-care can help replenish both the mind and the spirit and offer a protective barrier against depression.
- Abstinence
Alcohol use and drug abuse can trigger depression. Substances impact the reward systems in the brain that play a crucial role in the manifestation of adverse mental health symptoms. Drugs and alcohol influence the brain to produce an abundance of certain neurochemicals, such as dopamine and serotonin. When someone sobers up, the brain may have a difficult time producing these chemicals in the correct amount, which can manifest as depression symptoms. People with a genetic risk factor for major depressive disorder can lower their risk of experiencing a depressive episode by abstaining from drugs and alcohol.
There are no guarantees in life. Even with the best efforts, people with a genetic risk factor for major depressive disorder can develop the disease. Fortunately, depression is a treatable disorder. Most depression patients will favorably respond to antidepressant medications for depression.
But in cases where prescription drugs don’t work, non-invasive deep brain stimulation techniques like TMS are highly effective and safe for treating major depressive disorder.
Transcranial Magnetic Stimulation to Help with Possible Genetic Depression
Have you ever noticed that sometimes more than one person in a family suffers from a mental health disorder? Depression is one of the most common forms of mental illness. DNA can play a part when multiple family members are afflicted with any of the many forms of depression.
Genetic or environmental depression?
A study in the American Journal of Psychiatry found that depression tends to run in families. In fact, first-degree relatives of individuals with chronic depression are 2.52 times more likely to have depression themselves. One of the study authors commented that researchers have known for years that depression runs in families.
While it is known that depression tends to run in families, what is important to remember is that it may not be entirely due to genetics. Shared environmental factors can explain some of the depression risk among people who have close relatives with the condition. For instance, a 2014 study found that having a mother who lives with depression can place children at risk of emotional and behavioral issues. Due to these findings, it may not be that depression is passed through genetics, but having a parent with depression could result in a different home environment, which increases the risk of depression.
When people are related they tend to share experiences. Some of these experiences that they have in common may be the root of their depression. It can be difficult to determine. Some of these experiences include:
- Shared trauma such as a serious motor vehicle accident, home invasion, or physical attack.
- Family illness. Cancer in a loved one can cause depression in the rest of the family. The gravity of the disease can cause mental health issues such as depression, obsessive-compulsive disorder, or anxiety.
- Death of a loved one. This is one of the leading causes of depression.
Isolation and depression
Being isolated from other people due to illness or other reasons can cause depression and anxiety. The COVID-19 pandemic was a serious cause of depression for people due to being forced to isolate. This can happen if you totally isolate or if you are isolated from the rest of the world with other people.
A 2021 study in the Community Mental Health Journal evaluated rates of depression and anxiety around the globe during the COVID-19 quarantine period. Of 678 people who participated in the study, just over half showed signs of anxiety, and 58.6% had symptoms of depression. Study authors concluded that anxiety and depression were highly prevalent as a result of COVID-19 isolation. Study results also indicated that single and divorced people were likely to experience depression, as were unemployed and who did not get sufficient exercise. This study highlights that depression has causes aside from genetics, and if depression showed up in families during the pandemic, it could be due, at least partially, to the distress associated with the isolation and uncertainty.
The Interaction of Genes and Environment
While numerous risk factors can lead to depression, experts have generally concluded that genes and the environment interact to increase the risk of depression. There is not one single depression gene, but according to scientists writing for Frontiers in Psychiatry, multiple genes can increase the risk for depression. The disorder occurs due to an interaction of genetic and environmental risk factors. Genetics is believed to account for around 37% of the development of depression, but environment also plays a role, as genes on their own cannot explain the disorder.
Your chances of becoming depressed
The risk factors that can lead to a diagnosis of major depressive disorder can include:
- Mental health issues in blood relatives. The risk is higher though it is not always possible to know if a diagnosis of depression is truly due to genetics.
- Alcohol and other substance abuse.
- Financial problems.
- The weather. Long, unrelenting winters can cause seasonal affective disorder, which is also known as SAD. This can affect family members or just one person.
TMS Treatment for Depression, in a Safe Environment
If depression runs in your family, you may benefit from TMS, which is FDA-approved for treatment-resistant depression. Remember that chronic depression is likely to run in families, so those with relatives who have treatment-resistant depression are more vulnerable to the condition themselves. The research with TMS shows that it reduces depression symptoms more than a placebo, and patients who receive TMS are five times more likely to experience remission compared to those in a placebo group.
If you or a loved one is experiencing treatment-resistant depression, Pulse TMS is here to help. We continue to follow CDC guidelines in the aftermath of the pandemic, so we can assure you that treatment is provided in a safe environment. Contact us today to learn more.
Updated content on 7/16/2021

