OCD Guide
A Guide to Obsessive Compulsive Disorder Statistics and Treatment
Obsessive Compulsive Disorder (OCD) is a serious psychological issue that affects people of all demographics and socio-economic classes. OCD is an adverse neurological condition, affecting millions of men, women, and children worldwide. The disorder can be so disruptive if left untreated that it is in the top 20 causes of illness-related disabilities worldwide. Untreated OCD can lead to physical illness, and also cause depression and severe anxiety. The following guide will cover the demographic statistics, risk profiles, and current and effective treatment methods for Obsessive Compulsive Disorder.
What is Obsessive Compulsive Disorder?
The Diagnostic and Statistical Manual of Mental Disorders, or the DSM, provides psychologists and other mental health clinicians with official definitions, methods, and diagnostics for recognizing mental health and behavioral disorders. The DSM is currently in its fifth edition and illuminates the following clinical markers for OCD.
OCD happens when someone is preoccupied with a series of compulsions and obsessions. These obsessions and compulsions lead to anxiety and ritualistic actions and thinking patterns that can severely impact a person’s life. OCD rituals can take up a substantial amount of time, and mental and physical energy on behalf of the person affected. Individuals with OCD who are unable to perform a ritual, or compulsion, will experience anxiety and emotional disturbances that adversely impact their quality of life. Emotional distress from untreated OCD can also trigger clinical depression in vulnerable individuals.issue that affects people of all demographics and socio-economic classes. OCD is an adverse neurological condition, affecting millions of men, women, and children worldwide. The disorder can be so disruptive if left untreated that it is in the top 20 causes of illness-related disabilities worldwide. Untreated OCD can lead to physical illness, and also cause depression and severe anxiety. The following guide will cover the demographic statistics, risk profiles, and current and effective treatment methods for Obsessive Compulsive Disorder.

What are obsessions?
An obsession is a persistent and uncontrollable thought, image, or impulse. The person who experiences an obsession will find it unwanted, disturbing, and intrusive. Obsessions trigger distress in the person with OCD. To alleviate their suffering and dispel these negative images or thoughts, the individual will engage in a compulsion.
In most cases, people with OCD realize that their obsessions are irrational. But they can’t control them. The feelings obsessions trigger, such as disgust, doubt, or fear, are very real and intense. People who experience these obsessions are compelled to do something in a particular, and often a time-consuming way to alleviate these negative, intense and anxious feelings, even if they understand on an intellectual level that the obsessions and subsequent compulsions do not make any sense.
What separates OCD from an obsessive-compulsive personality trait is if the obsessions and compulsions disrupt activities that the person normally values. Also, most people will have intrusive thoughts from time to time. But what separates people with a clinical disorder from those who do not have a disorder is the level of anxiety those thoughts trigger. People with OCD cannot move on from intrusive thoughts. They are gripped with negative feelings and must engage in compulsions to dispel those feelings.
What is a compulsion?
A compulsion is a behavior that a person with disturbing obsessions performs to lessen their feelings of anxiety or distress concerning the obsession. Compulsions are often repetitive in nature. They aren’t always a physical action, either. In some cases, a compulsion could be a mental ritual that a person must engage in to alleviate their anxiety. For people who suffer from OCD, they believe that performing a compulsion is the only way to relieve their distress. Unfortunately, compulsions only reinforce the obsession, creating a cycle that worsens as long as the OCD remains unaddressed and untreated.
What are some examples of obsessions?
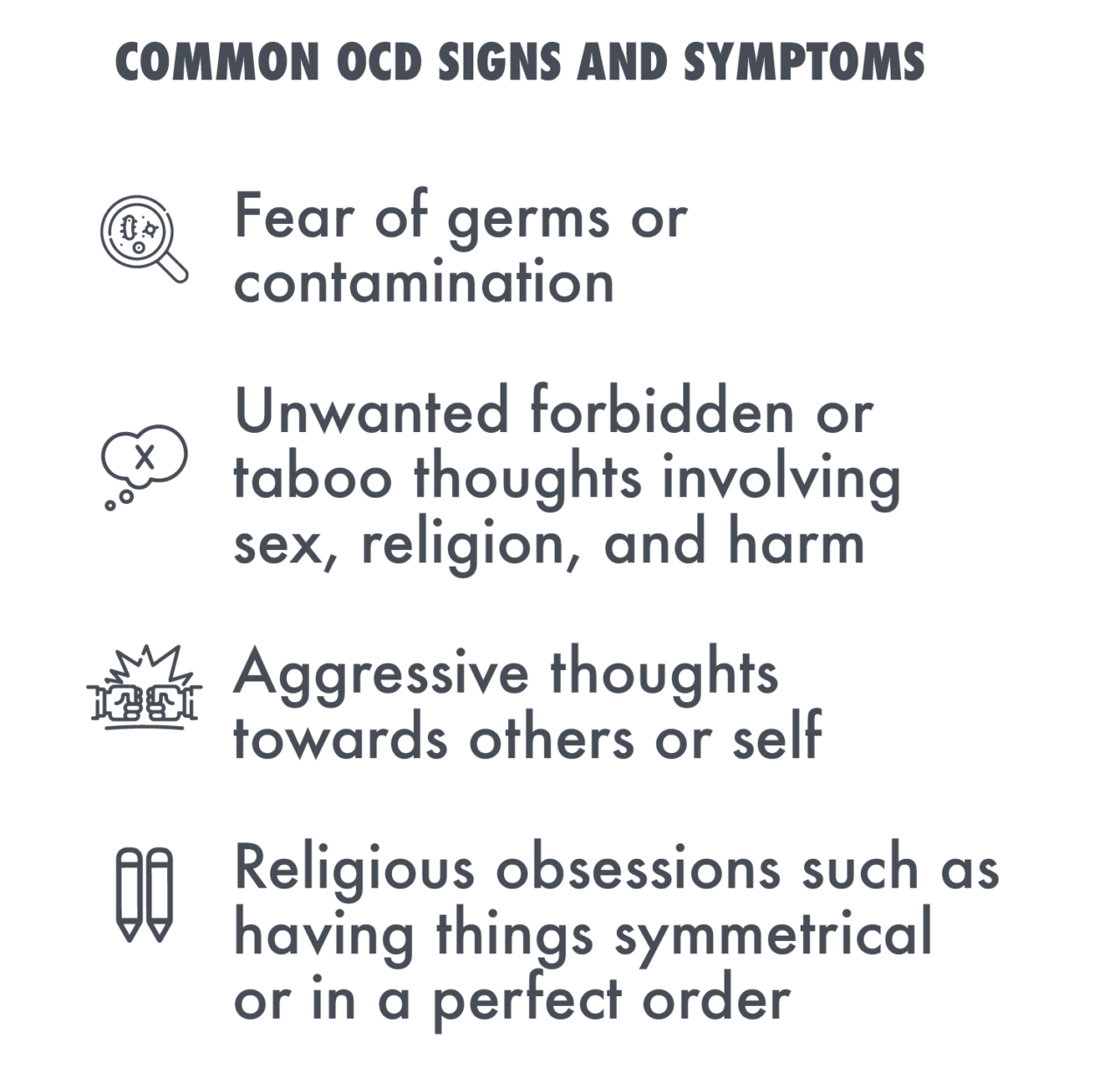
There are several common themes regarding obsessions and the compulsions in people with OCD.
- Contamination
Contamination from germs, bodily fluids, chemicals, dirt, and environmental pollutants is an extremely common obsession. People with OCD will fear infection or disease from certain triggers.
- Unwanted Sexual Thoughts
Intrusive, and disturbing sexual images are another common obsession with OCD sufferers. These obsessions can be incredibly debilitating, distressing, and embarrassing.
- Fear of Losing Control
Another marked feature in OCD obsessions is the fear of ‘losing control.’ People fear blurting out obscenities, lashing out physically, or engaging in other violent or socially deviant acts.
- Religious Obsessions
Some people with OCD may have a preoccupation with God or other religious themes. They may become obsessive about morality and fear committing blasphemous acts.
What are some common compulsions?
In cases of obsessions regarding contamination, many people with OCD will engage in ceremonial hand washing, bathing, or grooming techniques. They may clean their homes or other objects several times over if they fear their body or possessions are contaminated. These rituals can take up a lot of time and prevent people from engaging in valuable activities they may need to perform or otherwise enjoy.
OCD sufferers will often engage in repetitive behaviors, such as tapping a body part or repeating a word or an action to alleviate disturbing mental imagery. Counting while performing a task to a number that is deemed good or safe is another common compulsion. Sufferers may repeat certain body movements, such as waving their arms a certain way. They may have to put objects in order a specific way or touch something in a pattern to alleviate anxiety. In cases of religious obsessions, they may pray compulsively to prevent harm or something terrible from happening when triggered.

How does OCD interfere with someone’s life?
OCD can severely impact a person’s life in multifaceted ways. Left untreated, OCD can lead to other severe mental health conditions, such as anxiety and panic attacks, and depression. Untreated mental health conditions are also a significant source of drug and alcohol addiction. People will often turn to drugs or alcohol to cope with the distress of an untreated mental disorder. For people with OCD, compulsions can take up hours of a person’s time. They can miss school, work, and their personal and professional relationships can suffer under the weight of an untreated mental health condition.
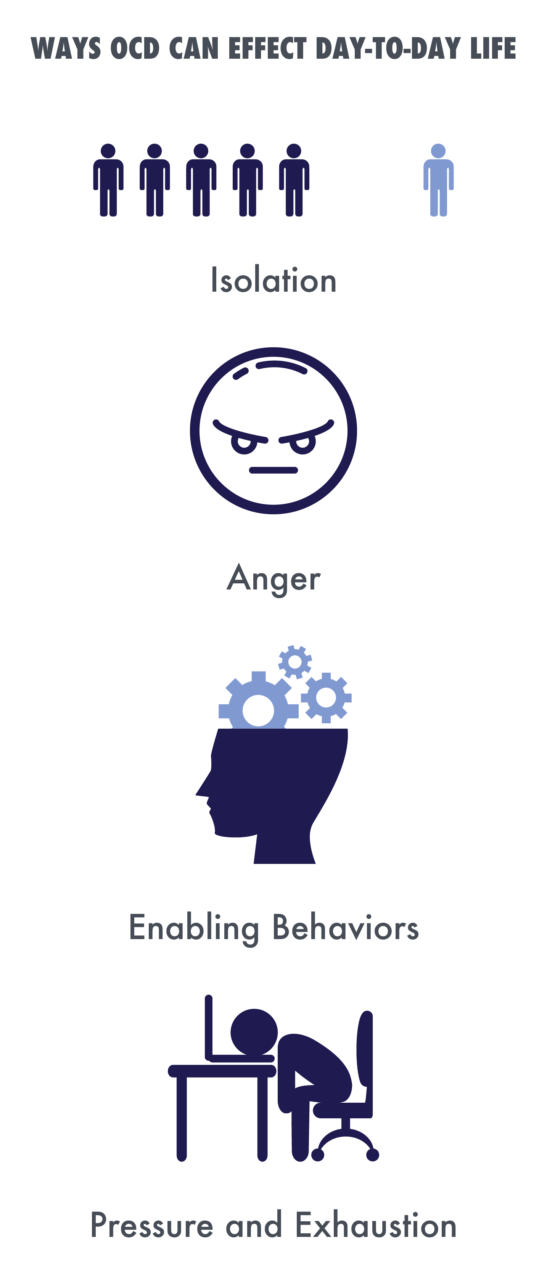
- People with untreated OCD often isolate themselves from others.
Intrusive, disturbing thoughts, and the pressure and subsequent exhaustion that a person feels after performing compulsions leads them to isolate themselves socially. Social isolation makes it harder for people to seek help from others and may prolong the negative impacts of the disease. OCD can also cause someone to avoid certain situations or places that can trigger an obsession. Isolation and loneliness can lead to depression. Suffering from untreated OCD can cause feelings of powerlessness, and loss of control.
- Anger
It is common for sufferers of OCD and their loved ones to experience anger related to the disorder. Family members and friends who do not understand the disease may blame the sufferer, which can also fuel the cycle of isolation, loneliness, and depression. Resentment on behalf of the sufferer and loved ones can also prevent the OCD sufferer from getting the help they need.
- Enabling Behaviors
For people with OCD, their family members may not understand that it is a treatable mental disorder. There is a risk that loved ones may engage in enabling behaviors. Enabling behaviors prevent the person with OCD from realizing how severe the condition is, and from seeking help. In these types of cases, family therapy can be extremely beneficial for breaking enabling behavior patterns and getting the OCD sufferer the support they need to manage the condition.
- Pressure and Exhaustion
The anxiety, pressure, and exhaustion inherent in OCD can lead to a host of physical health issues. For example, obsessive hand washing can cause skin irritation, or lead to a serious infection. OCD sufferers may wash their hair so frequently that they develop lesions or other scalp issues that can become infected. They may lose precious sleep performing rituals, which can negatively impact their immune system and cause their personal and professional life to suffer.
How does someone develop OCD, and who is most at-risk?
A combination of neurobiological, genetic, behavioral, environmental, and cognitive factors all influence the onset of OCD in vulnerable individuals. Recent studies on brain images of people with and without OCD indicate that OCD symptoms are a malfunction in communication signals between different areas of the brain. The areas most significantly affected are the orbitofrontal cortex, the anterior cingulate cortex, the thalamus, and the striatum. The neurotransmitters that send messages to these parts of the brain are also different in people with OCD. Dopamine, serotonin, and glutamate are all affected.
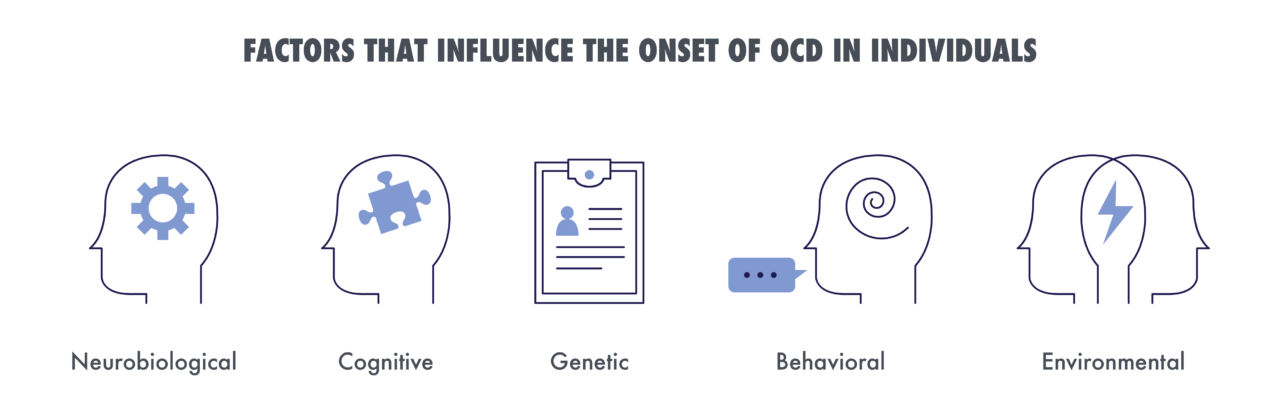
Traumatic brain injuries have been found to trigger OCD in some cases. Also, behavioral theorists suggest that people with OCD exhibit faulty belief systems that may contribute to the excessiveness of their compulsions. People who exhibit perfectionist behaviors, over-inflated levels of responsibility, and an intolerance for uncertainty are at higher risk of developing the disorder.
Genetics also play a role in the development of OCD. Variations in gene mutations and other genetic components can trigger the disorder. For example, up to 25% of OCD sufferers have a close family member with the disease. In twin studies, genetics contribute between 45 to 65% of the risk for exhibiting OCD symptoms.

Studies indicate that the onset of OCD typically starts during two age groups. OCD symptoms will manifest either between the ages of 8 and 12 or during the teens or young adult years.
- 2% of U.S. adults have OCD.
- Women have slightly higher rates of OCD than men.
- Lifetime prevalence of OCD rates is 2.3%
- Half of all adults with OCD experience significant impairment
- 35% of adults have moderate impairment
- 14% of adults with OCD have a mild impairment
- People between the ages of 18 – 29 have the highest levels of OCD
- 10% of OCD sufferers constantly question their sexuality as a part of the disease
How is OCD treated?
It is essential to treat OCD soon after it manifests. Without treatment, compulsions can become more pronounced and cause physical and other mental health problems. OCD is commonly treated with a combination of medication, cognitive behavioral therapy, and sometimes family therapy.
SSRIs are usually the first line of treatment for OCD.
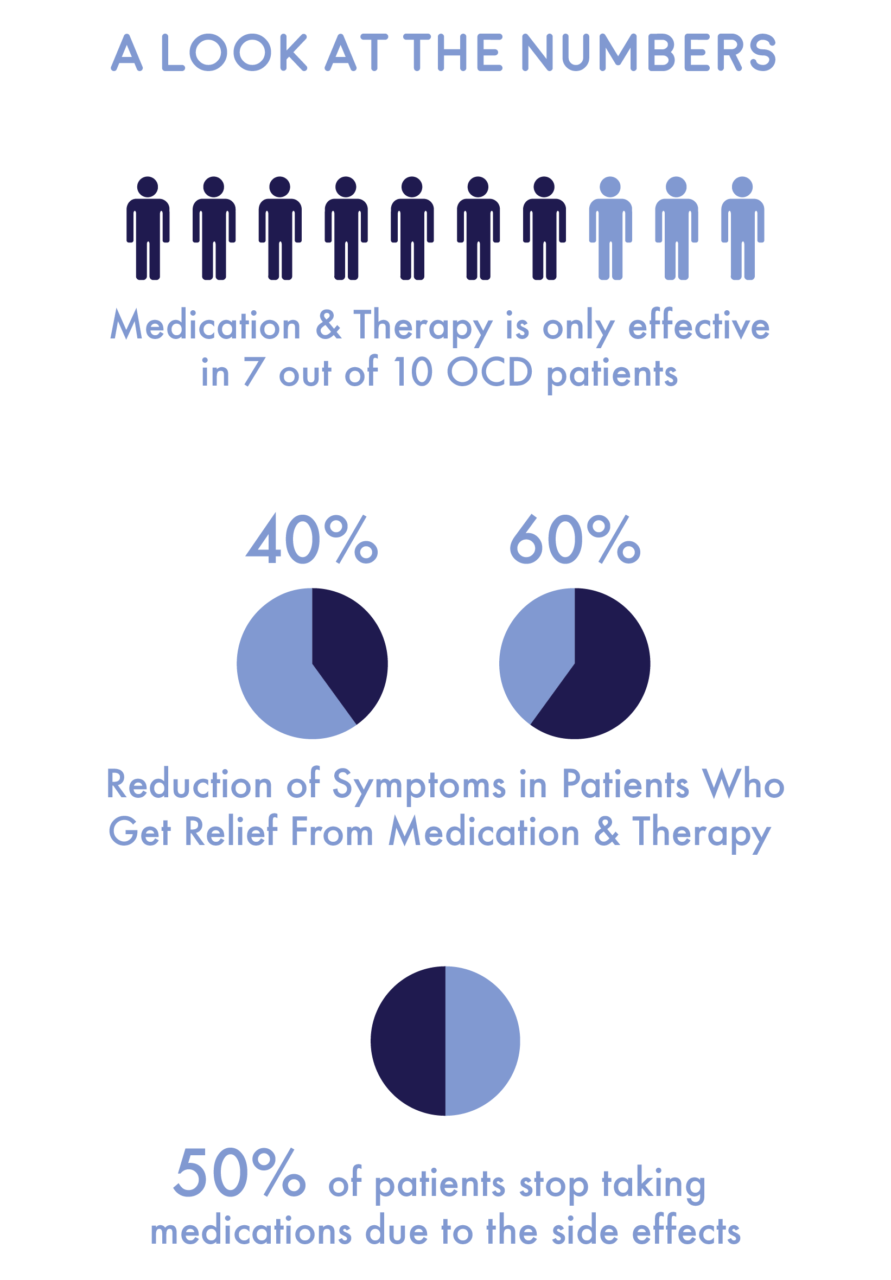
- 7 out of 10 OCD patients get relief from medication and therapy. They will see a reduction of symptoms between 40 and 60%.
- Half will stop taking medications due to the side effects. TMS and other deep brain stimulation techniques can help where medicine has failed.
OCD sufferers who haven’t been able to find a medication that is effective for them have found success with deep brain stimulation therapies, such as transcranial magnetic stimulation (TMS).
TMS uses an unobtrusive, powerful magnet to change the activity in certain, targeted areas of the brain. TMS helps to change the flow of information between neurotransmitters and neural pathways to alleviate obsessions, compulsions, and anxiety in OCD sufferers. TMS enables patients to live healthy and functional lives free of intrusive and distressing thoughts.
TMS treatment is an outpatient procedure that only takes about an hour to perform. Patients are awake during the procedure and can return to work and their normal activities soon after the session is completed. Sessions take place Monday through Friday from anywhere between three and six weeks depending on the severity of the patient’s OCD.
Studies indicate that most patients see an improvement in functioning and reduction in distressing symptoms after four weeks of TMS treatment. For most, improvements hold for up to four months. Not only do most TMS patients see a reduction in OCD symptoms, but they also experience a decrease in anxiety and depression symptoms as well.
Cognitive behavioral therapy and family therapy are effective at helping OCD patients and their loved ones develop healthy ways of minimizing the impact of obsessions and compulsions. CBT is effective for assisting individuals with ways to recognize and cope with OCD triggers. People who suffer from OCD usually do well with a combination of medication and therapy. SRIs and therapy are also effective at treating other issues associated with OCD, such as anxiety, panic attacks, and depression.
Left untreated, OCD can get worse. The symptoms can also lead to more serious mental health issues and physical side effects due to compulsions. Although OCD is a serious disorder, the condition responds well to a range of different treatment methods. For people who suffer from the condition, numerous foundations and organizations are dedicated to studying and treating OCD.